Virtual reality in pain management: theoretical and clinical exploration

Virtual reality use cases are not limited to video games and the entertainment industry. In recent years, the use of virtual reality has grown considerably in the medical sector, especially as a promising tool for the management of pain and anxiety.
Through this article, we will describe in a simplified way how virtual reality makes it possible to modulate the perception of pain. We will then present the most representative clinical studies as well as concrete practical applications. You will discover why and how this technology is positively impacting the lives of thousands of patients around the world.
Virtual reality: a powerful distraction from pain
To understand how pain is modulated, we will rely on Gate theory (“Gate control theory” in English), proposed by Ronald Melzack and Patrick D. Wall in 1965 [1], [2]. This theory suggests that there is a “gate system” in the spinal cord that makes it possible to decide whether pain signals are important enough to be transmitted to the brain. Several factors can influence the opening and closing of these doors:
- Signal strength: A stronger signal is more likely to pass through doors.
- Emotional state: Stress, anxiety, and fear can open doors and amplify pain.
- Medications: Some medications, such as painkillers, work by closing doors or blocking pain signals in the thalamus (a region in the brain involved in processing the pain signal).
- Distractions: When a sensory stimulus (tactile, auditory, visual, etc.) attracts our attention, it competes with the painful stimulus. These sensory stimuli reach the brain more quickly, which will impact the processing of the pain signal. In other words, the new stimulus “partially closes the door” to the pain signal, thereby reducing its perception.
In recent years, the use of virtual reality has become more widespread in the hospital sector, as headsets have proven to be particularly effective tools to act as a distractor to divert attention from pain. A neuroimaging study has also shown a reduction in the brain activity of regions involved in the perception of pain during virtual reality sessions (Figure 1) [3].

Why is virtual reality so effective in drawing attention away from pain? VR headsets have significant pain relieving potential, as they offer rich and engaging experiences that highly demand the attention skills of patients. The most effective experiences, such as those offered by Lumeen, incorporate several concepts to optimize the potential for distraction:
- Multimodal sensory stimulations: Headsets combine visual and auditory stimuli.
- Feeling of presence: allows the user to feel immersed in the virtual environment, as if they were actually there. It creates a more realistic and engaged experience.
- Captivating narratives: An engaging immersive scenario can transport the patient out of reality and absorb them into the story.
- Interactive activities: Integrating interactions and challenges into the VR experience encourages the patient to actively engage and focus their attention. This can include games, interactions with virtual characters, or dynamic environments.
- Medical hypnosis, cardiac coherence and music therapy : the integration of hypnotic verbal support, cardiac coherence exercises and soothing music makes it possible to act on the level of anxiety and pain.
Our Cayceo experiences combine all these concepts and even make it possible to trigger stimuli to amplify the diversion of attention at the fateful moment, when you are about to do an injection, a puncture, an incision... click here to learn more.
The gate theory, simplified in this article, makes it possible to understand that pain is not a simple passive perception, but a complex process that is influenced by physical and psychological factors. It is important to note that this theory was developed in 1965 and has since been extensively researched. More recent theories of pain take into account more complex mechanisms, but the fundamental idea of gates remains a useful tool for understanding pain modulation (see the “To learn more” section).
Virtual reality as a tool for managing pain during care: evidence and clinical applications
What does the research say?
Among the applications of virtual reality in health, distraction to reduce pain during hospital care has been the most studied in two decades. In 2000, Hoffman and his team, pioneers in this field, set out to explore the analgesic potential of virtual reality [4]. To do this, they offered 12 burn patients (21% of the body surface area affected on average) to participate in motor rehabilitation sessions with and without virtual reality. The virtual reality experience used in this study took the form of an interactive game called “Snow World”, plunging patients into a snowy environment in computer graphics. The results indicated a notable decrease in pain intensity in the immersive virtual reality condition compared to a condition without virtual reality. Other preliminary studies have demonstrated the effectiveness of virtual reality in reducing pain in patients undergoing medical procedures such as wound care and physiotherapy. In particular, these studies revealed that patients experienced a 35 to 50% reduction in pain during virtual reality sessions compared to the usual treatments without virtual reality [5].
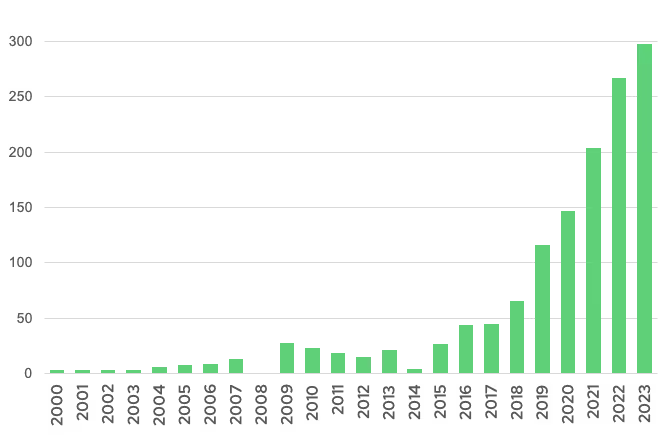
This first study by Hoffman and his collaborators contributed to the significant increase in research on virtual reality in the field of health, particularly over the last five years (Figure 2).
Subsequently, numerous studies looked at the benefits of virtual reality as a complementary non-pharmacological treatment for pain. Technology has been shown to be effective in reducing drug use in many care pathways, up to 40% of opioid use [6].
For children and adolescents, virtual reality has been evaluated for the management of pain in several contexts: dental care, burn care, oncology, injections (vaccines, blood tests, etc.). A systematic review and meta-analysis concluded that virtual reality used as a distraction during medical procedures in pediatrics provided effective management of patient-induced pain [7]. In adults, virtual reality is also widely used to relieve acute pain experienced during care procedures or during and after surgery. Used alone or in addition to an analgesic, immersive virtual reality has particularly proven itself in the case of wound and burn care and the insertion of needles and catheters [8].
Virtual reality can also help manage chronic pain. A 2021 literature review highlighted that this technology could be an alternative to painkillers in the management of back pain [9]. Another study involving 80 women with breast cancer showed that an immersive virtual reality session (used in addition to the use of morphine) significantly reduced chronic pain associated with cancer compared to using morphine alone [10].
Virtual reality and pain: applications in the medical sector
In the medical sector, virtual reality is currently used as a therapeutic tool for pain management in a variety of contexts:
- Chronic pain relief,
- Treatment of post-operative pain,
- Distraction during painful medical procedures, such as:
- Changing bandages, burns, or wounds
- Venous injections and injections,
- Dental care,
- Childbirths and other gynecological procedures,
- Certain surgical procedures (e.g. implantation of an implantable chamber, biopsy, bronchoscopy, etc.).
- During physiotherapy sessions, helping patients focus on specific movements while minimizing pain perception.
Note that there are also other use cases of virtual reality in the medical sector such as: the management of phobias, the training of caregivers, awareness-raising, therapeutic education as well as the alleviation of preoperative anxiety.
The take-home message
Virtual reality is emerging as an innovative and promising therapeutic tool in the fight against pain:
- By offering a non-drug alternative effective and beneficial for patients,
- En acting on the mechanisms of pain perception, it makes it possible to reduce the intensity of the pain experienced, to improve the comfort of patients and to reduce their use of painkillers,
- By proposing a field of application that extends to a wide variety of painful situations,
- By opening new perspectives in patient care through a therapeutic approach immersive, personalized, and engaging.
To learn more about our turnkey virtual reality solutions for pain management, visit our dedicated page.
To go further
Neurobiology of pain:
The gate theory:
The different theories of pain:
References
[1] R. Melzack and P. D. Wall, “Pain Mechanisms: A New Theory: A Gate Control System Modulates Sensory Input from the Skin Before It Evokes Pain Perception and Response.” Science, vol. 150, nO 3699, p. 971-979, nov. 1965, doi: 10.1126/science.150.3699.971.
[2] M. Moayedi and K.D. Davis, “Theories of Pain: From Specificity to Gate Control,” J. Neurophysiol., vol. 109, n.O 1, pp. 5‑12, Jan. 2013, doi: 10.1152/jn.00457.2012.
[3] H. G. Hoffman et al., “Modulation of thermal pain-related brain activity with virtual reality: evidence from fMRI”:, NeuroReport, vol. 15, n.O 8, p. 1245‑1248, June 2004, doi: 10.1097/01.wnr.0000127826.73576.91.
[4] H. G. Hoffman, D. R. Patterson, and G. J. Carrougher, “Use of Virtual Reality for Adjunctive Treatment of Adult Burn Pain During Physical Therapy: A Controlled Study”:, Wink. J. Pain, vol. 16, nO 3, p. 244-250, Sept. 2000, doi: 10.1097/00002508-200009000-00010.
[5] H. G. Hoffman et al., “Virtual Reality as an Adjunctive Non-pharmacologic Analgesic for Acute Burn Pain During Medical Procedures,” Ann. Behav. Med., vol. 41, nO 2, p. 183‑191, Apr. 2011, doi: 10.1007/s12160-010-9248-7.
[6] T. McSherry, M. Atterbury, S. Gartner, S. Gartner, E. Helmold, E. Helmold, D. M. Searles, and C. Schulman, “Randomized, Crossover Study of Immersive Virtual Reality to Decrease Opioid to Decrease Opioid Use During Painful Wound Care Procedures in Adults”:, J. Burn Care Res., p. 1, May 2017, doi: 10.1097/BCR.0000000000000589.
[7] R. Eijlers et al., “Meta-analysis: systematic review and meta-analysis of virtual reality in pediatrics: effects on pain and anxiety,” Anesth. Analog., vol. 129, n.O 5, p. 1344, 2019, doi: 10.1213/YEAR.0000000000004165.
[8] Q. Huang, J. Lin, R. Han, R. Han, C. Peng, and A. Peng, and A. Huang, “Using Virtual Reality Exposure Therapy in Pain Management: A Systematic Review and Meta-Analysis of Randomized Controlled Trials,” Value Health, vol. 25, n.O 2, p. 288‑301, Feb. 2022, doi: 10.1016/j.jval.2021.04.1285.
[9] C. Tack, “Virtual reality and chronic low back pain,” Disabil. Rehabil. Assist. Technol., vol. 16, nO 6, p. 637‑645, August 2021, doi: 10.1080/17483107.2019.1688399.
[10] E. Bani Mohammad and M. Ahmad, “Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: A randomized control trial,” Palliate. Bracket. Care, vol. 17, n.O 1, p. 29‑34, Feb. 2019, doi: 10.1017/S1478951518000639.
Photo credit: Coline Bachelier
Want to test Lumeen for 30 days with no commitment?